By Adityan, Editor, Soch Se
For over 100 million adults in India, life with diabetes is a daily battle. It’s a battle of blood sugar readings, dietary restrictions, and often, a heavy reliance on insulin. In recent years, a new class of “wonder drugs” like Ozempic and Mounjaro has emerged globally, offering incredible control over blood sugar. But for the vast majority of Indian patients, they remain a distant, unaffordable dream. What if, however, the most powerful solution wasn’t in an expensive, imported injection pen, but was already lying dormant inside our own bodies?
A groundbreaking study from Duke University has just uncovered a biological secret that could fundamentally reshape how we understand and treat diabetes. Researchers have found that the pancreas has a hidden backup system: alpha cells, long thought to only produce the sugar-raising hormone glucagon, can switch gears and produce GLP-1, the very hormone that makes drugs like Ozempic so effective.
From my perspective as the editor of Soch Se News, this isn’t just another piece of lab science. This is a story of immense hope, particularly for India. The real story isn’t that our bodies have an “Ozempic-like backup,” but that this discovery could pave the way for homegrown, affordable therapies that awaken this sleeping giant within our own pancreas. Could this be the key to loosening the grip of a disease that affects so many of our families? Let’s explore what this new alpha cells GLP-1 diabetes discovery truly means.
The Old Biology: A Tale of Two Cells
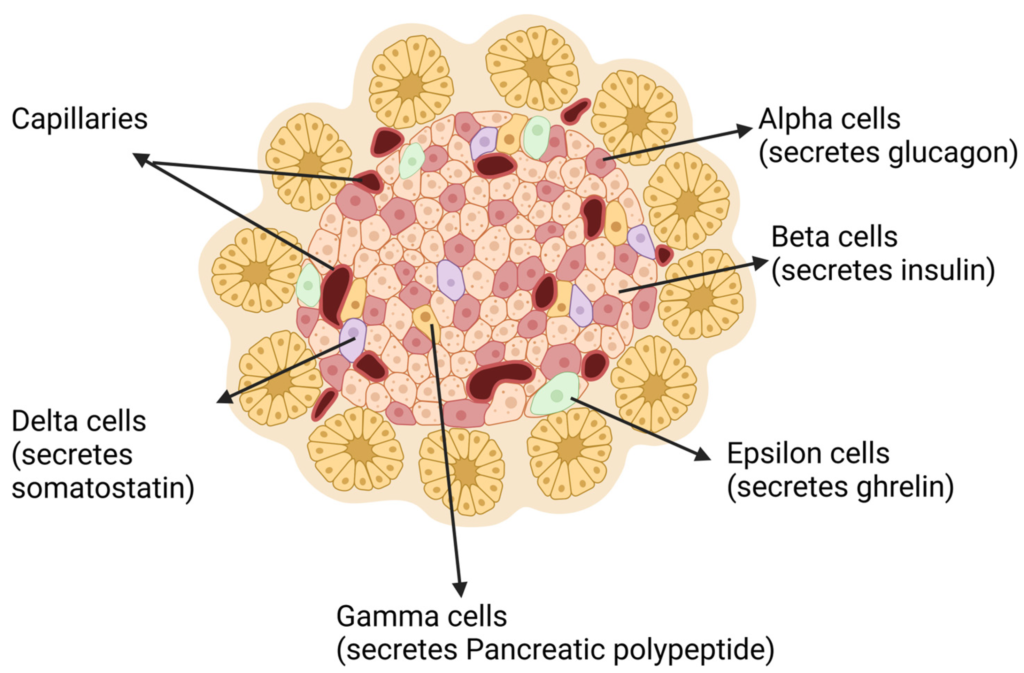
Before we dive into the new discovery, it’s important to understand the conventional wisdom that has defined diabetes care for decades. For years, scientists believed the pancreas’s blood sugar regulation was a simple tug-of-war between two key players in cell clusters called islets:
- Beta Cells: The heroes of the story. They produce insulin, the hormone that tells your body to absorb sugar from the blood, thus lowering blood sugar levels. In Type 2 diabetes, these cells either don’t produce enough insulin or the body becomes resistant to it.
- Alpha Cells: Traditionally seen as the antagonists. They produce glucagon, a hormone that does the opposite of insulin—it tells the liver to release stored sugar into the blood, raising blood sugar levels.
The goal of most diabetes treatments has been to either boost insulin’s effect or suppress glucagon’s. Then came GLP-1.
The Rise of GLP-1 and the “Ozempic” Revolution
GLP-1 (Glucagon-Like Peptide-1) is a powerful hormone produced in the gut that acts as a master regulator. It potently stimulates beta cells to release insulin when blood sugar is high, and it also suppresses the alpha cells’ production of glucagon. Drugs like Ozempic and Mounjaro are synthetic versions (analogues) of this hormone. They are incredibly effective but come with a staggering price tag. From my comparative analysis, Western trials show patients spending $800–$1,000 per month on these GLP-1 analogues. For the average Indian family, this is simply unsustainable. This is why the new discovery from Duke University is so profoundly important for us.
For a deeper understanding of our commitment to factual and ethical reporting, you can review our editorial policy.
The New Discovery: The Pancreas’s Hidden Superpower
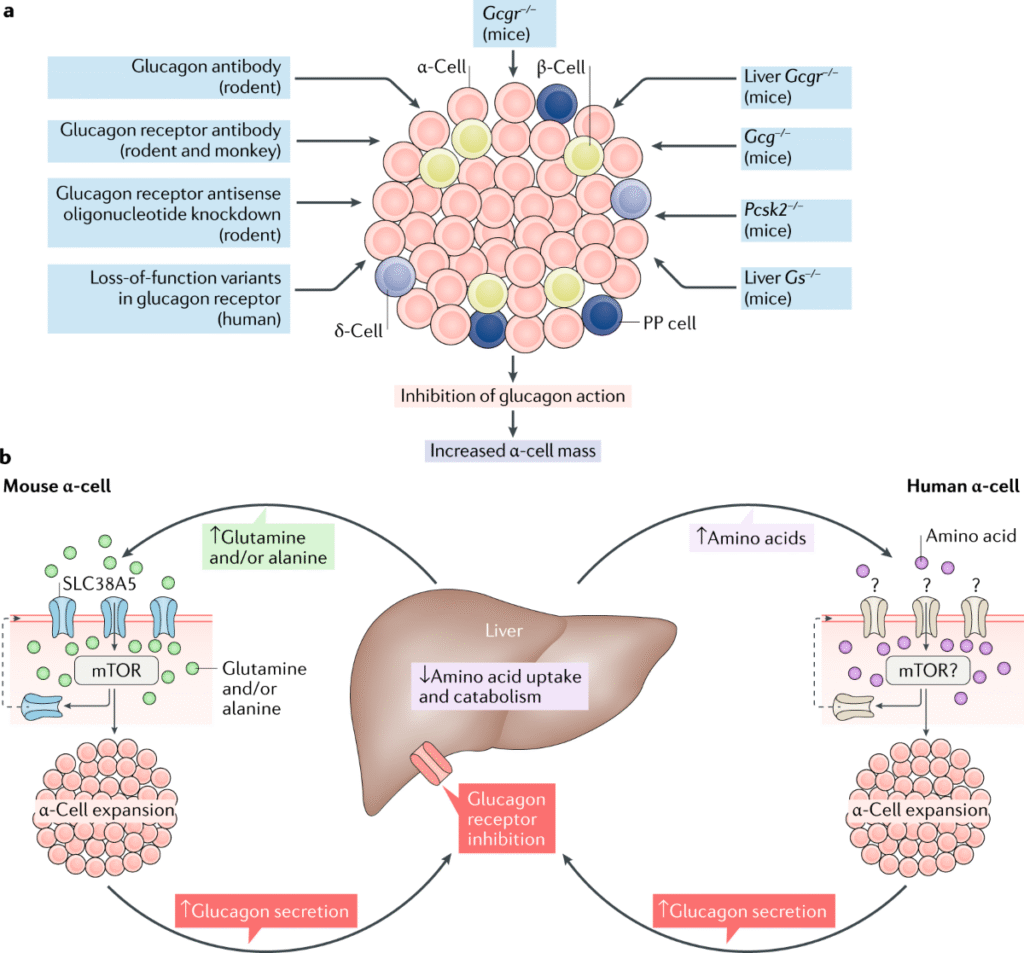
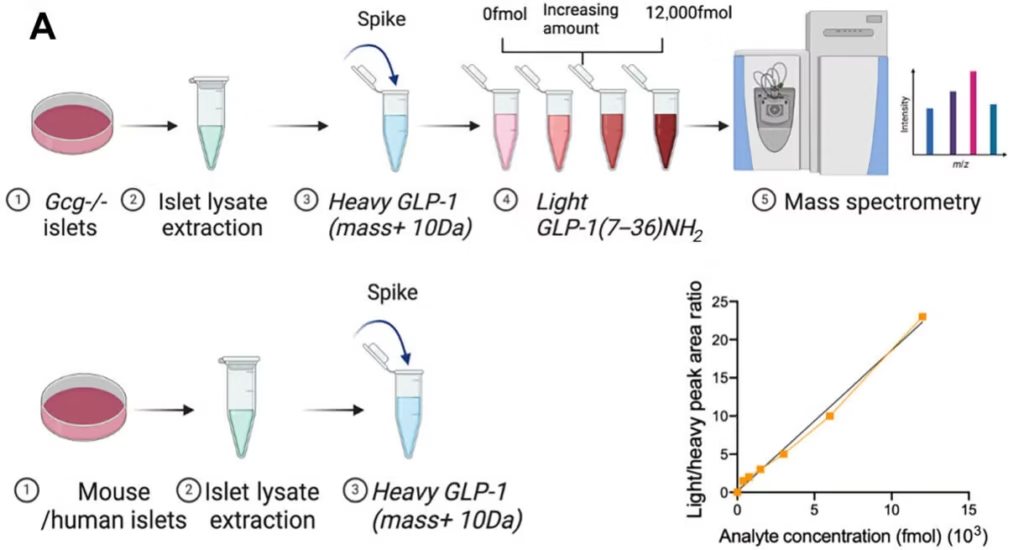
The Duke University research, published in a leading scientific journal, has turned the old biology on its head. Using advanced techniques, scientists discovered that alpha cells are not one-trick ponies. They have a hidden, dual-function capability.
At the heart of this discovery is a fascinating biological switch involving enzymes called convertases. Think of them as tiny molecular scissors inside the cell.
- Normally, an enzyme called PC2 is active in alpha cells. It snips a precursor molecule to produce glucagon.
- However, the researchers found that alpha cells also contain another enzyme, PC1/3. When this enzyme is active, it snips the same precursor molecule in a different spot, producing GLP-1 instead of glucagon!
This is the “convertase flip” that, from my perspective, could be the master key for next-generation therapies. By finding a way to encourage alpha cells to use the PC1/3 scissors more often, we could theoretically get the pancreas to produce more of its own GLP-1.
In-Depth Analysis: What This Means for India’s Diabetes Epidemic
This is where we connect the dots from the lab to our lives. What does this alpha cells GLP-1 diabetes discovery mean for the millions of Indians managing this chronic condition?
A Path Beyond Expensive Imports: The Affordability Angle
While Western media is framing this as an “Ozempic-like backup,” from my contextual opinion, the bigger story for India is affordability. Our nation is on track to become the world’s diabetes capital, with projections soaring past 130 million people in the coming years. If our own alpha cells’ GLP-1 production can be harnessed, we may be able to bypass the crippling reliance on Big Pharma’s injectable drugs, which are currently luxury medicines here. Imagine a future where a simple, affordable pill could “reprogram” your alpha cells. This could make effective GLP-1-based treatment 10 to 20 times cheaper in India, making it accessible to the masses, not just the wealthy.
Reducing Insulin Dependence for Millions
From my local research insight, this discovery is not just academic—it could translate into major policy shifts and pharmaceutical investments right here in India. Even a modest boost in endogenous (internally produced) GLP-1 could have a massive impact. Because local GLP-1 acts directly on its neighboring beta cells (a paracrine effect), it’s incredibly efficient at stimulating insulin secretion. For millions of Type 2 diabetics, this could mean a significant reduction in their dependence on external insulin injections, improving their quality of life and reducing the financial burden on our healthcare system.
The Future is Personalized: Could Treatment be Gender-Tailored?
One of the most intriguing findings from the research was an unexpected sex difference: pancreatic islets from females were found to produce significantly more GLP-1 than islets from males. This correlates with the known fact that women are generally more insulin-sensitive. This raises a fascinating question for the future of medicine in India. Does this open the door for gender-tailored diabetes therapies? Could treatments one day be adjusted based on a person’s biological sex to achieve the optimal GLP-1 response? It’s a tantalizing glimpse into a future of true precision medicine.
If you have questions about this analysis, please feel free to contact us.
The Road Ahead: From Discovery to Drug
It is crucial to manage expectations. This research is a monumental step, but it is the first step on a long road. My forward-looking statement is this: if validated in further human trials, this research could lead to the development of islet-targeted drugs that specifically boost local GLP-1 secretion. This would be a revolutionary step for precision medicine in India, especially for Type 2 diabetics who have become resistant to current drugs.
Major questions remain, such as how much this alpha-cell-derived GLP-1 contributes to overall systemic glucose control. But the door is now open. The focus of research will now shift from simply replacing GLP-1 to finding ways to awaken the pancreas’s own incredible, built-in capacity to produce it. We must, of course, provide a disclaimer that this is early-stage research and not yet a treatment.
Conclusion:
So, what is the ultimate takeaway from the groundbreaking alpha cells GLP-1 diabetes discovery? It is a story of profound hope. For decades, we have viewed the alpha cell as part of the problem in diabetes. Now, we see it may hold the key to the solution.
My final verdict is this: this discovery is more than just a scientific curiosity. It is a fundamental shift in our understanding of the pancreas and a beacon of hope for over 100 million Indians. It opens a tangible pathway toward developing affordable, homegrown therapies that could transform diabetes care in our country. It reminds us that sometimes, the most powerful solutions are not in a vial, but are already written into our own biology, waiting to be unlocked.
The journey from this discovery to a widely available medicine will be long, but for the first time, the destination seems within reach. To learn more about our mission to bring clarity to complex stories like this, please visit our about us page.
Frequently Asked Questions (FAQ)
1. Is this discovery a cure for diabetes?
No, this is not a cure. It is a fundamental biological discovery that opens up a new and very promising avenue for developing future treatments for Type 2 diabetes. It suggests we might be able to get the body to better regulate its own blood sugar.
2. How long will it be before this becomes a real treatment?
The journey from a basic science discovery to a clinically approved drug is typically very long, often taking 10-15 years of rigorous research, development, and clinical trials.
3. Does this discovery apply to Type 1 diabetes?
The immediate implications are primarily for Type 2 diabetes. In Type 1 diabetes, the body’s immune system destroys the insulin-producing beta cells. While enhancing GLP-1 could still have some benefits, the core problem of missing beta cells remains, making this discovery less directly applicable than it is for Type 2.